Table of Contents
Jennifer Frederick was in the best form of her life in 2023, so when she felt a little bump in the area of the groin after a week of training. She thought it was just a fired muscle, but a month later, the bump was still there.
Four months later, the bump increased. Frederick went to a dermatologist and the tests found more songs in the leg. She has planned a biopsy. On December 14, surgeons cut her leg and removed the biggest pieces. A week later, she had a diagnosis: clever metastatic melanoma. The disease is generally announced by a mole on the skin, but Frederick has never had one.
More tests have shown that cancer was not only in its leg. A scan found four lesions on his lungs. Another has found five lesions on his brain. The results were shocking, said Frederick.
“I have never had a migraine, headache, blurred vision, never had any problems to breathe, never had a cough,” said Frederick, 50. “I never felt at all.”
Jennifer Frederick
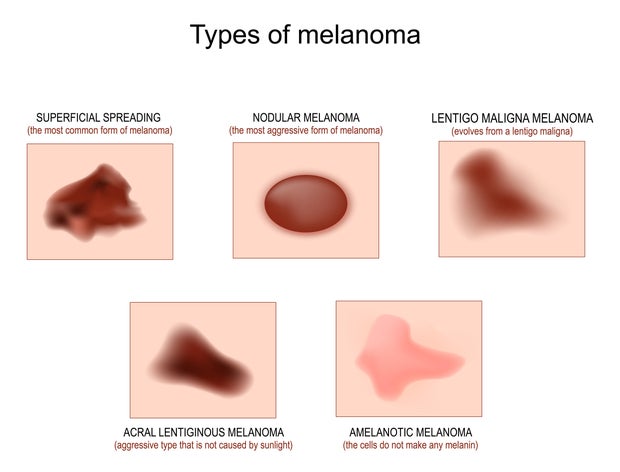
What is metastatic clever melanoma?
Melanoma is the deadliest form of skin cancer. Metastatic melanoma is at any time of cancer melanoma which has spread from one place to another, said Dr. Michael Postow, a medical oncologist at the Memorial Sloan Kettering, who was not involved in the treatment of Frederick. Mecal metastatic melanoma Referring to metastatic melanoma at an advanced stage.
“Melanoma is a kind of cancer that can spread quite largely throughout the body,” said Postow. “This is one of the cancers that frequently involves the brain, therefore distributed from melanoma to the brain … can be quite common. The lung is also a common site of metastatic melanoma.”
As a rule, melanoma is recognized by a brown or a black Taupe on the skin. Postow said he was unusual but not unknown for a patient not to have a mole or “microscopic”. He said that in addition to keeping an eye on a new mole or an existing mole that changes color, size or texture, people should monitor the pieces under the skin like the one Frederick had. Any concern should be brought to a dermatologistSaid Postow.
Zhabska T. / Getty Images
The five -year survival rate for advanced metastatic melanoma patients is around 35%, according to The American Cancer Society. Postow said show clinical trials That for patients who receive certain immunotherapy treatments, this number amounts to 50%. A decade ago, the five-year survival rate was closer to 10%, he said.
Immunotherapy was what Frederick’s doctor, the Cleveland Clinic medical oncologist, Dr. Lucy Boyce Kennedy, recommended. The two talked about the options and decided to go with an intensive treatment that would combine the radiation of gamma knives and two immunotherapy drugs. Kennedy described the treatment protocol as “a fairly high risk” and warned that it could lead the immune system to attack other organs. Frederick was not discouraged.
“She explained what it was going to look like. And I looked at her and said:” I don’t care what it is. If it is the most aggressive treatment, I am ready to do anything “,” said Frederick. “I just wanted to be my healthy Jen Frederick again so that I can resume a normal life.”
Difficult treatment
Frederick suffered Gamma knife radiotherapy January 7. The treatment uses precise gamma rays to target cancer tumors. Frederick said it went well, but when she started to receive immunotherapy medication every two weeks on January 17, she began to feel “bad side effects”, including “pseudo-Grippal symptoms, rash, nausea” and high fevers.
As it continued treatment, side effects developed to include vomiting, chills and problems with its stomach and eyes. She used the bathroom “more than 25 times a day,” said Frederick. She was hospitalized and spent a month in and outside the hospital. There was significant inflammation in its colon. She weighed only 95 pounds.
Jennifer Frederick
“They would free me. I would go home. I would be at home 24 hours and I should go back because I would start to vomit. I could not remember food,” said Frederick. She had to take two months of leave from immunotherapy to take steroids, antibiotics and other drugs to treat side effects. After recovering, she resumed the treatment.
When Frederick has undergone his first TEP since the start of treatment, it showed “a major and major improvement,” she said. It made the months of pain, discomfort and illness were worth it. A second scan several weeks later showed that things continued to move “in the right direction,” said Frederick. Immunotherapy was reduced every three weeks, then every four weeks while it continued to improve.
“My doctor said I’m a stadium miracle,” said Frederick.
“Cancer did not have me”
After 18 months of treatment, Frederick saw no progression of his cancer and continues to improve, said his care team. Kennedy believes that she has “a very excellent chance of having long -term survival”. Clinical trials Patients who received the same treatment as Frederick has done is still doing 10 years after the study, According to a recent updateSaid Kennedy. She thinks Frederick will have a similar journey.
“I only use the number of 10 years because it is just as old as drugs. I think these patients will have answers that would have more than that, potentially indefinitely,” said Kennedy.
Jennifer Frederick
Frederick will continue his treatment until December 2025, said Kennedy. Then she will start to undergo regular screening analyzes to ensure that her cancer does not come back. Frederick said that once she has finished with active treatment, she wants to share her story and make sure people know the importance of early screening. It began to supervise other patients with cancer through the 4th Angel Program of the Cleveland Clinic.
“I want people to know that it becomes more difficult before it is easier,” said Frederick. “My saying has always been” I may have cancer, but cancer doesn’t. “And I want people to feel in this way, because it is not a death sentence.”